Dr Foued Ben Romdhane
Written By Kelly M. Pyrek Published on infectioncontroltoday.com
Standard precautions (SPs) are one of the cornerstones of infection prevention and control, designed to limit bloodborne pathogen exposures among healthcare workers (HCWs) and halt the transmission of healthcare-associated infections (HAIs) to patients. To review, the components include hand hygiene, use of appropriate personal protective equipment (PPE), safe use and disposal of sharps, decontamination of environment and equipment, patient placement, and linen and waste management
There is new thought that compliance with SPs is part of the overall safety of culture cultivated within healthcare institutions. Zingg, et al. (2015) identified the critical elements of effective infection-prevention programs in hospitals and key components for implementation of monitoring, and found that appropriate use of guidelines as well as multimodal and multidisciplinary prevention programs (including behavioral change, engagement of champions, and positive organizational culture) were instrumental.
Studies have indicated a less than 50 percent adherence rate; the reasons for this suboptimal adherence to SP is underexplored, say Hessels, et al. (2016), who sought to explore the relationships among safety climate factors and SP adherence by healthcare personnel in hospitals using newly developed survey and observational tools.
The researchers collected data from 11 units in five hospitals, where a patient safety and standard precaution survey was administered to nurses and pooled with data from observations of HCW/patient interactions using defined SP indications. Among the 540 HCW/patient encounters with 1,713 SP indications and 140 surveys collected, most nurses (94 percent) reported always or often adhering to SPs and generally re-ported positive scores on unit safety climate. However, the observed SP adherence was 62 percent; only 30 percent of nurses rated staffing positively, and this was inversely related to observed SP adherence.
As Hessels, et al. (2016) observe, "Similar to other studies, we found hand hygiene was performed around half of the time when indicated and was more often missed prior to patient contact than after patient contact. Notably, one-quarter of the time when hand hygiene was missed, the HCW was wearing gloves, even when gloves were not indicated. We also found on the other hand that donning gloves or gowns when indicated did not occur during 13 percent and 43 percent of observed encounters, respectively." They add, "Appropriate donning of masks and sharps and linen handling were also suboptimal. These findings are concerning given the high burden of HCW sharps injury and bloodborne pathogen exposures, transmission risks of epidemic concern, such as influenza, and in the context of accruing evidence of the importance of environmental cleanliness to prevent the spread of healthcare-associated infection." The researchers emphasize that measuring SP adherence and associated factors using reliable and valid observation and survey tools will allow healthcare administrators and infection preventionists to both target local interventions and measure and benchmark progress internally and externally to improve SP adherence.
Some researchers have explored the barriers to SP adherence, including de Carvalho Nagliatea, et al. (2013) who say that factors include lack of motivation, lack of knowledge of technical staff, insufficient qualification of professionals, work overload, lack of orientation for healthcare professionals to address difficulties to use SP in practice and inappropriate behavior of more experienced professionals negatively influencing other team members. Additionally, Efstathiou, et al. (2011) found that reported factors were lack of knowledge, lack of time, forgetfulness, lack of means, negative influence of the equipment on nursing skills, uncomfortable equipment, skin irritation, lack of training, conflict between the need to provide care and self-protection, and distance to necessary equipment or facility.
Powers, et al. (2016) say that despite published guidelines on infection control and negative health consequences of SP noncompliance, significant issues remain around SP adherence to protect nurses from bloodborne infectious diseases, including hepatitis B virus, hepatitis C virus (HCV) and HIV.
The researchers conducted a descriptive correlational study of 231 registered nurses working in ambulatory care that measured self-reported compliance with SP, knowledge of HCV, and perceived susceptibility and severity of HCV plus perceived benefits and barriers to SP use. They found that fewer than one-fifth (17.4 percent) of respondents to a questionnaire reported compliance with all nine SP components. The re-searchers also identified a significant relationship between susceptibility of HCV and compliance and between barriers to SP use and compliance. As Powers, et al. (2016) note, "Understanding reasons for noncompliance will help determine a strategy for improving behavior and programs that target the aspects that were less than satisfactory to improve overall compliance. It is critical to examine factors that influence compliance to encourage those that will lead to total compliance and eliminate those that prevent it."
Some experts emphasize the importance of education and training on standard precautions in nursing schools, and there are a handful of studies examining nursing students' SP compliance.
For example, Colet, et al. (2016) surveyed 250 nursing students in a cross-sectional, self-reported study. The majority were females (61 per-cent), single (79.7 percent), enrolled in the regular BSN program (65.3 percent), registered in the final year of the program (53.4 percent), and had attended training or seminars regarding infection control in the last 12 months (88.1 percent). According to the researchers, the students reported highest compliance in disposing of used sharp articles and instruments into sharps-only boxes, with a compliance rate of 84.3 percent, followed by decontaminating hands immediately after removal of gloves (compliance rate, 78 percent), washing hands between patient con-tacts (compliance rate, 75.8 percent), changing gloves between each patient contact (compliance rate, 74.2 percent), and wearing a surgical mask alone or in combination with goggles, face shield, and apron whenever there was a possibility of a splash or splatter (compliance rate, 72.9 percent). On the other hand, three of the items in the scale received a compliance rate of below 50 percent. The lowest compliance rate was reported in the item on using water only for handwashing (compliance rate, 26.7 percent), followed by placing waste contaminated with blood, body fluids, secretion and excretion in red plastic bags, irrespective of the patient’s infective status (compliance rate, 48.3 percent), and not recapping used needles after administering an injection (compliance rate, 49.2 percent).
Cheung, et al. (2015) conducted a cross-sectional survey study guided by the health belief model. There were 678 questionnaires analyzed, with a response rate of 68.9 percent. The mean frequency score of SP compliance was 4.38 out of 5. Year 2 and year 4 students had better SP compliance than year 3 students, and further analysis identified an interaction effect of perceived influence of nursing staff and year of study. The researchers identified five predictors for SP compliance: knowledge of SPs, perceived barriers, adequacy of training, management support, and influence of nursing staff. They say that "SP compliance among nursing students can be enhanced by increasing SP knowledge, providing more SP training, promoting management support, reducing identified SP barriers, and improving nursing staff compliance to SPs."
Livshiz-Riven, et al. (2014) conducted a prospective cohort study in which two consecutive classes of a four-year bachelor of nursing program completed questionnaires three times. Factor analysis displayed two behavioral categories: commonly used standard precautions (CUSPs) and less commonly used standard precautions (LUSPs). Knowledge, risk perception, sense of coherence (SOC), safety climate (SC), and emphasis given by educators were evaluated as associated factors. Of the 91 students, 85 (93 percent) completed the questionnaire during their second year, 57 of 88 students (65 percent) completed it during the third year, and 70 of 82 students (85 percent) completed it at the end of the fourth year. Of the 82 students, 45 (55 percent) completed three measurements. CUSPs exhibited a rise from the second to the third year, with a moderate decline from the third to the fourth year, whereas LUSPs continued ascending. CUSPs were positively associated with SC and SOC; LUSPs were commonly associated with risk perception.
In working with nursing students, Kim and Oh (2015) found a number of psychological barriers to SP adherence, such as worrying about patient discomfort, dealing with their own immaturity and fear, being emotionally uncomfortable, and feeling overwhelmed by tasks. Most participants shared that their SP compliance training during their clinical rotations was limited to following the lead of their nursing supervisors. Kim and Oh (2015) remind us that the Theory of Planned Behavior (TPB) explains that attitudes are influenced by intention and perceived control, and intentions are influenced by psychosocial determinants such as attitudes and subjective norms: "Unlike other social cognitive models in infection control area (e.g., health belief model, health locus of control, protection motivation theory), the TPB emphasizes predictors related to individual intention for behaviors. Since the TPB tests intentions towards specific infection control measures, such as understanding compliance with hand hygiene recommendations or physicians' intention to wear gloves during patient care, it is perceived as the best theory for explaining why healthcare workers do not follow SP compliance even though they have greater knowledge and cognitive awareness about the importance of it. In addition, the TPB considers the individual intention as a strong determinant in behaviors such as compliance."
Kim and Oh (2015) emphasize that "Although students participating in the study had learned about SP in their fundamentals of nursing and microbiology classes, most did not know much about the purpose and importance of SP. This is consistent with previous studies that found SP knowledge in nursing students to be relatively low. Participants reported confusion about the concept of SP and general infection control. Aware that they are at risk for pathogen exposure in clinical practice, students did not have a strong understanding of protection as a core concept of SP. The fact that students are aware of the risk of exposure to pathogens but less familiar with the SP guidelines means that students do not know how to protect themselves from the risk of exposure."
They add, " Nursing students' experiences of noncompliance are quite different from those of nurses due to the relatively low status of students within the information hierarchy. Students are not able to control resources and barriers within their working environments during their clinical rotations. In particular, participants experienced the absence of positive subjective norms and the presence of various barriers that need to be removed … The SP compliance demonstrated by healthcare workers, particularly nurses, affects students' perceptions and behaviors during clinical training. In previous studies, the reasons for SP noncompliance given by nurses included the following: lack of time, puts patients at risk, lack of means, precautions not warranted, interferes with patient care, forgetfulness, lack of knowledge and distance to necessary equipment or facility. Interestingly, most of this study's participants witnessed SP noncompliance by nurses in the general ward. Participants said that some nurses admitted to their noncompliance and then explained what they should follow as guidelines to the students. Others were not even aware of their noncompliance behaviors. These situations imply that students are in inappropriate or negative educational situations."
The noncompliance of healthcare workers as a cause of noncompliance of students is a significant problem noted by Erasmus, et al. (2009), who stated that their study's results indicate that beliefs about the importance of self-protection are the main reasons for performing hand hygiene. A lack of positive role models and social norms may hinder compliance."
As Kim and Oh (2015) emphasize, "Nursing students are the nurses of the future, so compliance education and a student's intention to follow compliance are directly related to a nurse's commitment to compliance." It's clear from a number of other studies that continued education and training is necessary for improved SP compliance.
Xiong, et al. (2016) sought to assess the effectiveness of a mixed media education intervention to enhance nursing students' knowledge, attitude and compliance with SPs. A randomized controlled trial with 84 nursing students was conducted in a teaching hospital in China. The intervention group (n = 42) attended three biweekly mixed media education sessions, consisting of lectures, videos, role-play, and feedback with 1 to 20 minutes of individual online supervision and feedback sessions following each class. The control group learned the same material through self-directed readings. Pre- and post-test assessments of knowledge, attitudes, and compliance were assessed with the Knowledge with Standard Precautions Questionnaire, Attitude with Standard Precautions Scale, and the Compliance with Standard Precautions Scale, respectively. The Standard Bacterial Colony Index was used to assess handwashing effectiveness. At the six-week follow-up, performance on the Knowledge with Standard Precautions Questionnaire, Attitude with Standard Precautions Scale, and Compliance with Standard Precautions Scale were significantly improved in the intervention group compared with the control group. The hand hygiene standard in the intervention group (38 passed) outperformed the control group (23 passed) (P < .01).
References:
Cheung K, Chan CK, Chang MY, Chu PH, Fung WF, Kwan KC, Lau NY, Li WK, Mak HM. Predictors for compliance of standard precautions among nursing students. Am J Infect Control. 2015 Jul 1;43(7):729-34. doi: 10.1016/j.ajic.2015.03.007. Epub 2015 Apr 11.
Colet PC, Cruz JP, Alotaibi KA, Colet MK and Islam SM. Compliance with standard precautions among baccalaureate nursing students in a Saudi university: A self-report study. Journal of Infection and Public Health. 2016.
de Carvalho Nagliatea P, Nogueirab PC, de Godoyb S and Costa Mendesb IA. Measures of knowledge about standard precautions: A litera-ture review in nursing. Nurse Education in Practice. Vol. 13, No. 4. Pages 244-249. July 2013.
Erasmus V, Brouwer W, van Beeck EF, Oenema A, Daha TJ, Richardus JH, et al. A qualitative exploration of reasons for poor hand hygiene among hospital workers: lack of positive role models and of convincing evidence that hand hygiene prevents cross-infection. Infect Control Hosp Epidemiol, 30 (2009), pp. 415–419 http://dx.doi.org/10.1086/596773
Efstathiou G, Papastavrou E, Raftopoulos V and Merkouris A. Factors influencing nurses' compliance with Standard Precautions in order to avoid occupational exposure to microorganisms: A focus group study. BMC Nursing. January 2011.
Hessels AJ, Genovese-Schek V, Agarwal M, Wurmser T, Larson EL. Relationship between patient safety climate and adherence to standard precautions. Am J Infect Control. 2016 Oct 1;44(10):1128-1132. doi: 10.1016/j.ajic.2016.03.060. Epub 2016 Jun 15.
Kim KM and Oh H. Clinical Experiences as Related to Standard Precautions Compliance among Nursing Students: A Focus Group Interview Based on the Theory of Planned Behavior. Asian Nursing Research. Vol. 9, No. 2. Pages 109-114. June 2015.
Livshiz-Riven I, Nativ R, Borer A, Kanat-Maymon Y and Anson O. Nursing students' intentions to comply with standard precautions: an explor-atory prospective cohort study. Am J Infect Control. 2014 Jul;42(7):744-9. doi: 10.1016/j.ajic.2014.04.002. Epub 2014 May 22.
Powers D, Armellino D, Dolansky M and Fitzpatrick J. Factors influencing nurse compliance with Standard Precautions. Am J Infect Control. 2016 Jan 1;44(1):4-7. doi: 10.1016/j.ajic.2015.10.001.
Xiong P, Zhang J, Wang X, Wu TL and Hall BJ. Effects of a mixed media education intervention program on increasing knowledge, attitude, and compliance with standard precautions among nursing students: A randomized controlled trial. Am J Infect Control. 2016 Dec 13. pii: S0196-6553(16)31015-X. doi: 10.1016/j.ajic.2016.11.006.
Zingg W, Holmes A, Dettenkofer M, Goetting T, Secci F, Clack L, Allegranzi B. Magiorakos AP and Pittet D. Hospital organization, manage-ment, and structure for prevention of health-care-associated infection: a systematic review and expert consensus. The Lancet Infectious Diseas-es. Vol. 15, No. 2, PP. 212–224. February 2015
The World Health Organization (WHO) released the "Global Guidelines for the Prevention of Surgical Site Infection." These new guidelines include 29 concrete recommendations to address the spread of infections and avoid superbugs that account for more than 400,000 extra hospital days and place patients at risk. Infection preventionists are encouraged to become familiar with the recommendations in these guidelines.
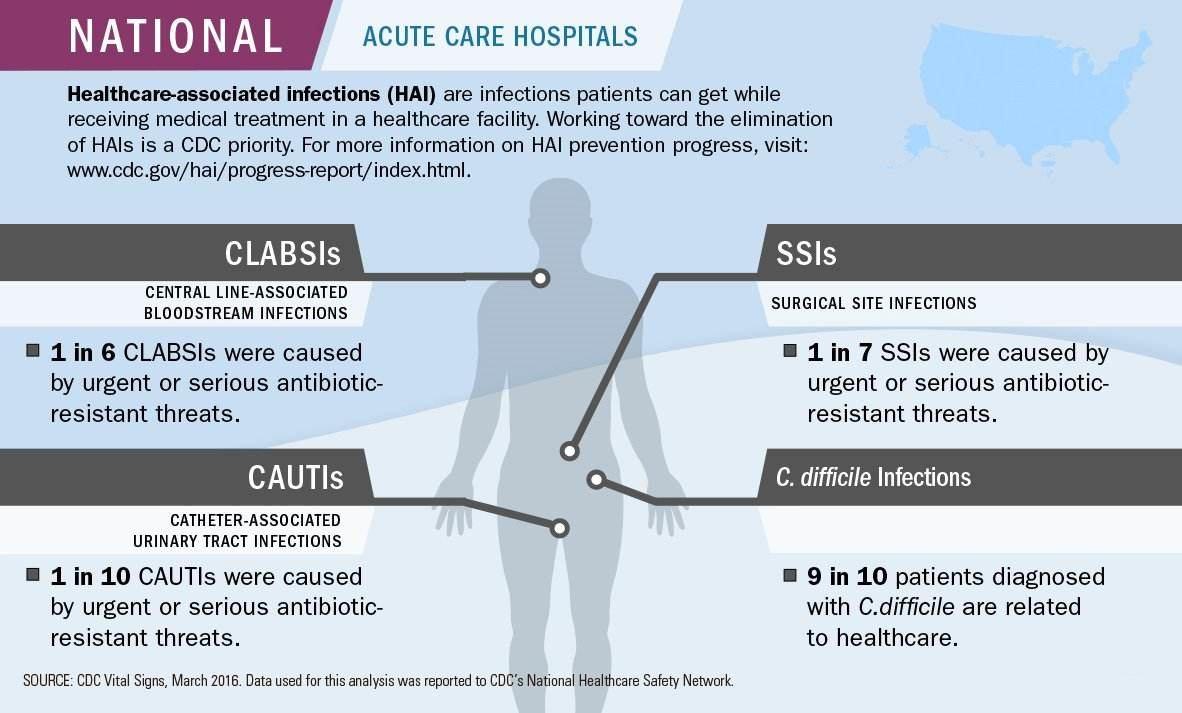
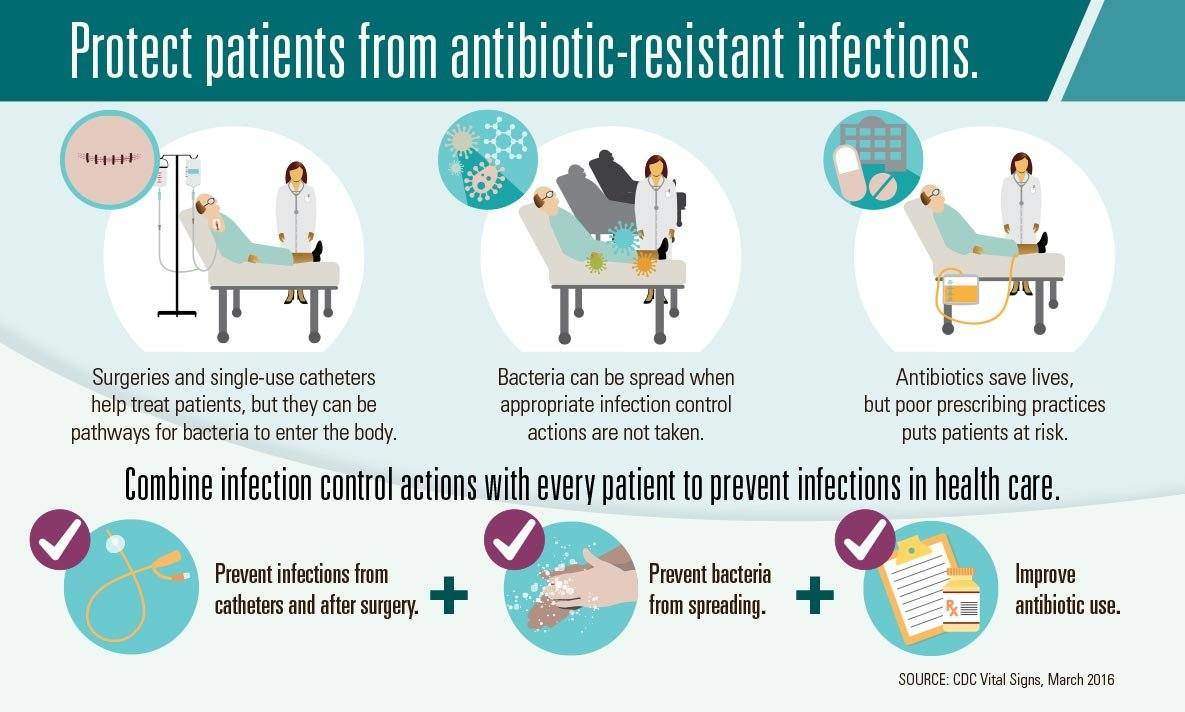
People receiving medical care can get serious infections called healthcare-associated infections (HAIs), which may lead to sepsis or death. Hospitals report common HAIs to CDC, including infections caused by C. difficile, infections following surgery, and infections following placement of a tube in the bladder or a large vein (catheter). These infections can be caused by bacteria that are resistant to antibiotics, making them difficult to treat. In certain kinds of hospitals, one in four of these infections (not including C. difficile) are caused by antibiotic-resistant bacteria identified by CDC as urgent or serious threats to health.* Although progress has been made, more work is needed. Three critical efforts to prevent an HAI are 1) prevent infections related to surgery or placement of a catheter, 2) prevent spread of bacteria between patients, and 3) improve antibiotic use. It’s important that healthcare providers take these actions with every patient every time to prevent HAIs and stop the spread of antibiotic resistance.
This is the latest Infection Prevention and Control Guidelines for Middle East Respiratory Syndrome Coronavirus (MERS-CoV) Infection.
5th Edition April 2018
Health care facilities should trace all health care workers who had protected or unprotected contacts with patients with suspected, probable, or confirmed MERS-CoV infection.
a) Testing (Nasopharyngeal swabs) for MERS-CoV is recommended even if asymptomatic.
b) Testing should not be done before 24 hours of exposure.
c) Single test only required unless symptomatic where repeated testing is required.
d) Contact should be off work until the test is reported as negative.
a) Testing for MERS-CoV is not recommended if asymptomatic.
b) Continue to work in the hospital unless they become symptomatic.
a) Testing for MERS-CoV is not recommended if asymptomatic.
b) Continue to work in the hospital unless they become symptomatic.
a) Patients can be exposed to MERS patients during pre-diagnosis phase or due to failure of recommended isolation precautions.
b) Testing for MERS-CoV should be done 24 hours or more after the last exposure.
c) Such patients should be followed for symptoms for 14 days after exposure with testing to be done upon development of symptoms suggestive of MERS.
The infection control unit of the facility or equivalent there of should trace all contacts within the HCF and proactively call by phone all contacts to assess their health daily for a total of 14 days. Contacts should also be instructed to report immediately to the Staff Health Clinic or Emergency Room if they develop upper or lower respiratory illness.
a) Investigation should be under guidance of Infection Prevention and Control Unit of the hospital, Regional Command and Control Center and Central Command and Control Center.
b) More testing of asymptomatic HCW may be required.
c) Cohorting or closure of units should be in consultation with the regional command and control center.
d) Surge plan to be in place in case of large outbreak.
Lorem ipsum dolor sit amet, consectetuer adipiscing elit. Aenean commodo ligula eget dolor. Aenean massa. Cum sociis natoque penatibus et magnis dis parturient montes, nascetur ridiculus mus. Donec quam felis, ultricies nec, pellentesque pretium quis, sem. Nulla consequat massa quis enim. Donec pede justo, fringilla vel, aliquet nec, vulputate eget, arcu. In enim justo, rhoncus ut, imperdiet a, venenatis vitae, justo.
One morning, when Gregor Samsa woke from troubled dreams, he found himself transformed in his bed into a horrible vermin. He lay on his armour-like back, and if he lifted his hea.
Lorem ipsum dolor sit amet, consectetuer adipiscing elit. Aenean commodo ligula eget dolor. Aenean massa. Cum sociis natoque penatibus et magnis dis parturient montes, nascetur ridiculus mus. Donec quam felis, ultricies nec, pellentesque pretium quis, sem. Nulla consequat massa quis enim. Donec pede justo, fringilla vel, aliquet nec, vulputate eget, arcu. In enim justo, rhoncus ut, imperdiet a, venenatis vitae, justo.
One morning, when Gregor Samsa woke from troubled dreams, he found himself transformed in his bed into a horrible vermin. He lay on his armour-like back, and if he lifted his hea.
- Cras dapibus Vivamus elementum semper.
- Maecenas odio ante tincidunt tempus.
- Donec sodales sagittis magna consequat.
- Integer ante accumsan a consectetuer.
- Nunc nonummy metus Vestibulum pretium.
- At solmen va esser necessi far uniform
- Li nov lingua franca va esser plu
- Lingues differe solmen in li grammatica
- When she reached the first hills
- Cozy sphinx waves quart jug of bad milk.

A wonderful serenity has taken possession of my entire soul, like these sweet mornings of spring which I enjoy with my whole heart. I am alone, and feel the charm of existence in this spot.
Lorem ipsum dolor sit amet, consectetuer adipiscing elit. Aenean commodo ligula eget dolor. Aenean massa. Cum sociis natoque penatibus et magnis dis parturient montes, nascetur ridiculus mus. Donec quam felis, ultricies nec, pellentesque pretium quis, sem. Nulla consequat massa quis enim. Donec pede justo, fringilla vel, aliquet nec, vulputate eget, arcu. In enim justo, rhoncus ut, imperdiet a, venenatis vitae, justo.
One morning, when Gregor Samsa woke from troubled dreams, he found himself transformed in his bed into a horrible vermin. He lay on his armour-like back, and if he lifted his hea.
- Cras dapibus Vivamus elementum semper.
- Maecenas odio ante tincidunt tempus.
- Donec sodales sagittis magna consequat.
- Integer ante accumsan a consectetuer.
- Nunc nonummy metus Vestibulum pretium.
- At solmen va esser necessi far uniform
- Li nov lingua franca va esser plu
- Lingues differe solmen in li grammatica
- When she reached the first hills
- Cozy sphinx waves quart jug of bad milk.

A wonderful serenity has taken possession of my entire soul, like these sweet mornings of spring which I enjoy with my whole heart. I am alone, and feel the charm of existence in this spot.
Lorem ipsum dolor sit amet, consectetuer adipiscing elit. Aenean commodo ligula eget dolor. Aenean massa. Cum sociis natoque penatibus et magnis dis parturient montes, nascetur ridiculus mus. Donec quam felis, ultricies nec, pellentesque pretium quis, sem. Nulla consequat massa quis enim. Donec pede justo, fringilla vel, aliquet nec, vulputate eget, arcu. In enim justo, rhoncus ut, imperdiet a, venenatis vitae, justo.
One morning, when Gregor Samsa woke from troubled dreams, he found himself transformed in his bed into a horrible vermin. He lay on his armour-like back, and if he lifted his hea.
- Cras dapibus Vivamus elementum semper.
- Maecenas odio ante tincidunt tempus.
- Donec sodales sagittis magna consequat.
- Integer ante accumsan a consectetuer.
- Nunc nonummy metus Vestibulum pretium.
- At solmen va esser necessi far uniform
- Li nov lingua franca va esser plu
- Lingues differe solmen in li grammatica
- When she reached the first hills
- Cozy sphinx waves quart jug of bad milk.

A wonderful serenity has taken possession of my entire soul, like these sweet mornings of spring which I enjoy with my whole heart. I am alone, and feel the charm of existence in this spot.